Here’s how to create a one-day pediatric foot-screening clinic at your own office
BY LOUIS J. DECARO, DPM
There are millions of parents out there who are concerned about how their child runs or walks. The problem for you is that they are told by countless professionals to do nothing, or sometime worse, they are referred to the wrong specialist. The problem is that most childhood foot deformities and abnormal biomechanics are ignored unless they are severe in nature.
Some pediatricians feel the children will “grow out of it” and that what they are experiencing are “growing pains.” Sadly, most people do not “grow out” of their foot problems, and those “growing pains” are actually a treatable foot issue.
We know that there are many parents harboring concerns about their child’s feet. What many do not know is that, besides their child’s complaint of discomfort, earlier and more obvious signs of biomechanical dysfunction may affect endurance or stability. The warning signs often observed by parents or healthcare professionals may be an antalgic gait, difficulty with walking/running, clumsiness, etc. Consultations with healthcare professionals may result in a variety of recommendations, ranging from custom orthoses to a simple prognosis that the child will outgrow the condition. While trying to remain clinically objective, it is important to “put yourself in the parent’s shoes.” When parents see their child struggling and dealing with pain or discomfort, being told, “s(he) will outgrow it” is often not an acceptable answer.
Another factor to consider when treating pediatric feet is the initial cost of custom foot orthoses—outgrowth and replacement on a regular basis during growth and development may be prohibitive to many family budgets. With parents looking for help, they will welcome the opportunity to have their children’s feet examined by a professional, followed by a prescribed treatment path. The children’s clinic opens the door to treat many candidates for potential orthotics in a single day. Following the foot exam, you will recommend appropriate treatment that may include custom or pre-fabricated foot orthoses.
Developmental Flatfoot
Developmental flatfoot is one of the most common conditions affecting the musculoskeletal system of children and teenagers. There is a tendency to under-treat or ignore a child’s flatfoot unless it is severe. Developmental flatfoot is the precursor to serious foot dysfunction and often results in some level of disability in the adult foot. Recognizing this anomaly early in life can prevent joints and musculoskeletal issues later in life.
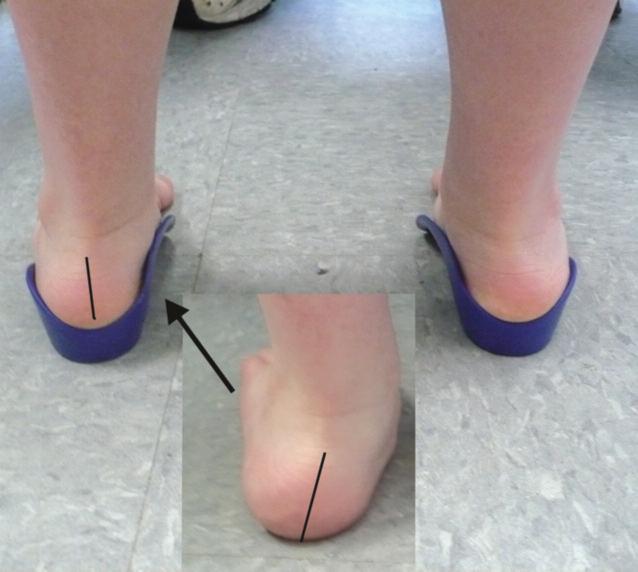
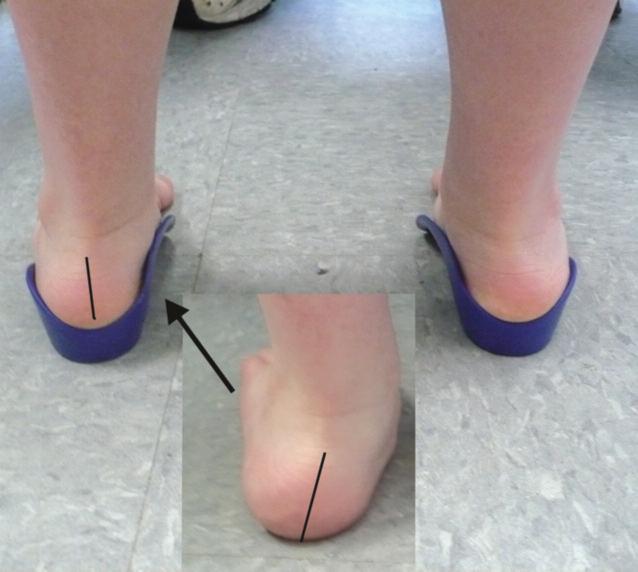
For age ranges 1-4 years old, a child most likely will have a flatfoot. This is considered normal. The two treatable “foot” issues for this age range, whether or not a flatfoot is involved, are a) the degree of calcaneal valgus or heel eversion and/or b) the milestone/gross motor impairment created from a poor foot type/egregious flatfoot causing ankle instability. A child with a significant finding of calcaneal eversion will severely toe out walk and will look
like he or she has a collapsed ankle and severe flatfoot. Most often, the parent will note a coordination issue, postural issues, and/or trouble progressing with ambulatory milestones. In addition, if the child has a significant amount of heel eversion or valgus, a child’s core strength may be inhibited. This can impede a child’s normal milestone gross motor development. A child may be doing early intervention but since the foundation is so or, the PT may not “stick” as well as if a child has a better-supported foundation. This “foundation” (or orthotic) is usually temporary and used to achieve more rapid gross motor achievement.
For age ranges 4-10, a child’s foot should not have a flatfoot appearance. This is an important message to impart to parents. A child in this age group who stands with a flatfoot should be treated with an orthotic. Once again, just like in a younger child, flatfeet at this age may not present with pain. Typically, pain is a rare symptom of a poorly functional foot type between the ages of 4-10. More commonly, children will experience balance, coordination, stural, or strength issues.
As early as 4 years old, kids will begin to show their disinterest in running sports. They may not know why they don’t “like” running sports, but they do know that their body is at a Figure 2: A Pediatric patient is observed during a
screening clinic. disadvantage. A thorough history of the “social choices” a child makes is an important part of the evaluation process. At this age, orthoses mostly still control the heel valgus and should only be rearfoot posted. The forefoot is still in its “formative stages”.
For kids 10 through 12 years old, an over-the-counter deep heel cupped orthotic is a great tool to have at a screening. Orthoses should incorporate a deep heel cup, high medial and lateral flange, medial rearfoot posting. and a medial skive. You can show kids and parents instantly what good foot correction looks like. If a child exhibits a rotational deformity, gait plates are also available over-the-counter to demonstrate to patients.
Once a child hits the age of 10, we as clinicians cannot necessarily treat kids as adults, but most of the time the child’s foot type can be grouped into its final adult foot type category. We know that genetic makeup dictates a large component of one’s foot type. There are a variety of foot types, but in general, all foot types can be sorted into six major categories. It is important to know exactly what foot type is involved before orthoses are prescribed. Each foot orthosis should be designed specifically for one’s foot type. In some cases, one’s left and right foot may not have the same foot type, and you will need two different types of orthoses.
The Quadrastep system of foot typing (www.thequadrastepsystem .com) is an easy-to-use tool for determining which of the six foot types your patient has. This system will allow you to meet all of your patients’ orthotic needs, particularly when patient finances are an issue. Additionally, patients can leave the clinic wearing these prefabs, immediately benefiting from the clinic. Alternatively, casts can be made during the clinic for those patients who cannot be fitted with prefabs, and can return at a later time for final fitting. In addition to a day filled with dispensing orthotics, you will add to your list of recurring patients who will seek your attention for many years to come.
Here is a quick how to:
Pre-Planning
Pre-Planning involves a series of steps to plan and prepare for a successful clinic:
• Pick a mid-week date that will include hours after 5 PM for working parents, or consider a Saturday.
• Be sure ample staffing is available to call on if needed.
• Have enough prefabs in stock to dispense during the clinic. Always have at least a sample of each size to try on.
• Be prepared to cast or scan during an exam.
• Set a date with at least 4 weeks advance notice.
Notification
Getting the word out to the public is a necessity! There are many potential avenues of promotion. Some are simple and can be activated immediately. Don’t assume, just because you are running a clinic, parents will find out on their own and show up. Keep promotional announcements brief and to the point, expressing FREE foot exam for Kids. Examples include:
• Use newspaper Ads. Cost-effectiveness will vary based on location.
• Mail postcards to your patient list: Keep it brief and to the point.
• Distribute flyers in local supermarkets, children’s stores, etc. with tear off tabs.
• Set up a registration page on your website. Be sure to emphasize that walk-ins are okay.
• Use hometown websites (patch.com may be helpful, depending on availability and local usage).
• Referring Health Professionals (local pediatricians, other MDs, DPMs, PTs, etc.).
• Leave information in local children’s stores.
At your office facility, use signage, take home reminders, mentioning at desk (do you know about our upcoming Kids Clinic?) Have your staff ask adult patients if they have kids or grandkids that might benefit from the upcoming free foot exam. Set up registration by calling a number, or going to a registration web page. For call-ins, try to schedule an appointment to manage patient flow. Walk-ins should be accepted but reservations will get preference for a free exam.
Clinic Day
Be sure your receptionist is prepared to welcome clinic parents. Have a registration sheet handy for contact information that includes the question, “how did you hear about the clinic?” This will tell you about the effectiveness of each notification method. Be sure to get e-mail addresses. Since there will be walk-ins, have staff on notice that they may be called for assistance. Have brochures or an overview sheet in the reception areas for those waiting.
Follow-Up
• Be sure to contact each parent attendee within a week following the clinic, by phone or email.
• Get opinions to help improve the next clinic…. would they attend again, what day/time of day would have been better, etc.?
• Start building a parent database for the future. You may want to schedule a Children’s Clinic on a regular basis (monthly, quarterly, etc.) and if you save contact information on an ongoing basis, your email and mailing database will become an effective promotional tool.
• Remember, children who start using orthotics early will return for next sizes several times, and will eventually become part of your adult patient base.
Foot Screening Process
Your initial exam may be exactly what you typically perform on a daily basis with your patients who come to you with complaints of biomechanical foot pain or gait abnormalities. Of course, this will include discussing with the parents or guardians their primary concerns that prompted their appointment with you. Some of the more common conditions you are going to be presented with in children under the age of 10 are flexible pes planus, developmental flatfeet, “growing pains/tendinitis”, and Severs. The majority of these conditions can often be treated with a pre-fabricated device that offers a deep heel cup with a few degrees of medial posting and skive.
Starting with the size based on foot/shoe size of your patient, you can simply check the fit to the foot just as you would a custom device with the end of the shell just proximal to the apex of the 1st MPJ for maximal control. Adolescents from the age of 10 and up have often developed their adult foot type and have completed any de-rotation that is going to occur within the foot. At this age and foot size, the patient may be ready for fitting with prefabs such as the QuadraStep adult orthotic system. The system will allow you to fit most feet from the most severe cavus foot type to the most over-pronated foot type. With a quick weight-bearing screening, looking at features such as medial longitudinal arch height, toesign and angle of gait, you can quickly narrow your orthotic selection down.
In summary, these complimentary pediatric screening clinics can increase your patient base for years to come, create “families” of patients, allow you the opportunity to dispense prefabricated devices on the spot creating an increased cash flow, create opportunities for an “outgrowth program”, and will earn you recognition as a pediatric specialist in your community.